Constant weighing and calculating food, ongoing worry, uncertainty, feelings of fear, and sleep interrupted by fright. These are just some of the problems faced by parents of children with Type 1 Diabetes. Every day, right after waking up, thoughts about glycemic levels and the uncertainty of whether their child will wake up at all cloud their minds… Is there anything that can alleviate this fear and slightly improve the life quality of a parent with a diabetic child? Certainly, knowledge that each of them must possess to properly care for their child is crucial. One of the key aspects related to this disease is a proper diet and administering the correct insulin doses. Feeding a child with Type 1 Diabetes is not easy, but it is something that can be learned.
POSSIBLE CAUSES AND SYMPTOMS OF TYPE 1 DIABETES
Type 1 Diabetes is an autoimmune disease caused by the failure of beta cells in the pancreatic Islets of Langerhans, which, when attacked by antibodies, lose the ability to produce insulin. The progressing deficiency, and consequently the absence of insulin, leads to hyperglycemia, which is responsible for the symptoms of diabetes. Type 1 Diabetes accounts for about 10% of all diabetes cases and affects roughly 1 in 1,000 children in developed countries. Formerly known as juvenile diabetes, it is now also diagnosed in adults.
The most common symptoms of Type 1 Diabetes in children include: drowsiness, lack of energy and appetite, sudden and excessive thirst, weight and muscle mass loss, frequent urination with a large volume of urine, the smell of acetone in exhaled breath, abdominal pain and vomiting, fever, consciousness disturbances, and in the most severe cases, loss of consciousness.
The causes of Type 1 Diabetes are not fully understood. It is not a hereditary disease. However, there are certain genetic predispositions and environmental factors that may be closely associated with its occurrence. The disease likely begins long before the first symptoms appear, and its progression is impossible to stop. Prevention of Type 1 Diabetes is virtually impossible, although recent scientific reports speak of administering probiotics to children at risk of developing the disease within the first 27 days of life to reduce autoimmunization.
Factors Associated with the Onset of Type 1 Diabetes
Genetic:
- Class II HLA genes (about 40%),
- Insulin gene (about 10%) and CTLA-4 (about 10%).
Environmental:
- Viral infections (enteroviruses, mumps, measles, Coxsackie),
- Vitamin D3 deficiency,
- Introduction of foreign proteins into the diet during early childhood,
- Additives of preservatives and colorants in food products,
- Stress, experienced traumas,
- Microbiota disturbances,
- – Antibiotic therapy.
Antibodies Attacking the Pancreas
- przeciwciała przeciwwyspowe,
- Antibodies against glutamic acid decarboxylase (70-80%),
- Anti-insulin antibodies (adults < 10%, children about 50%),
- Antibodies related to insulinoma-2 (about 60%).
DIAGNOSIS
The diagnosis of Type 1 Diabetes is based on randomly measured glycemia (twice equal to or higher than 200 mg/dl), immunological and biochemical tests, as well as the occurrence of clinical symptoms. Measurements of glucose (from a vein), glycated hemoglobin HbA1c test (an indicator of diabetes management and reflecting the average blood glucose level over the last 3 months), urine glucose and acetone concentration tests, C-peptide levels in the blood (indicating the pancreatic islets’ ability to produce insulin), and antibody concentration tests are performed.
In Poland, additional tests are conducted in children to check for diabetes complications and coexisting diseases. The most common among Type 1 Diabetes patients are celiac disease and Hashimoto’s autoimmune thyroiditis.
COURSE OF THE DISEASE
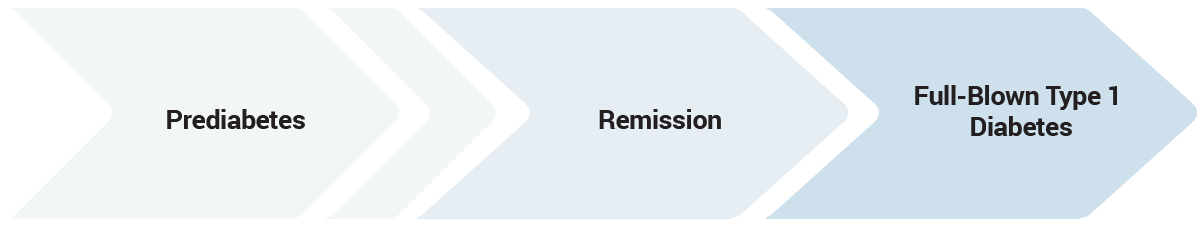
The course of Type 1 Diabetes can be divided into pre-diabetes (prediabetes), remission period, and full-blown Type 1 Diabetes. In the prediabetes phase, we deal with the appearance of antibodies associated with the destruction of pancreatic β cells. When about 90% of the pancreatic islet β cells are destroyed, the first symptoms of Type 1 Diabetes appear.
Remission usually begins after the initiation of insulin therapy when the calmed body starts to use the last reserves of its own insulin. During this time, patients take smaller doses of insulin, and sometimes they don’t take it at all. The remission period is often referred to as the “honeymoon phase,” preceding full-blown Type 1 Diabetes, which as a chronic disease, remains with the patient for life. The duration of remission often depends on a proper diet and healthy lifestyle. Unfortunately, even sudden, severe stress or infection can end it.
In full-blown, chronic Type 1 Diabetes, the health and functioning of the patient depend on the supply of external insulin for life. At this stage, the life of the patient and their family must be completely changed and reevaluated. The family learns to live with a new, serious, and chronic illness.
NUTRITION IN TYPE 1 DIABETES
Contrary to appearances, nutrition in Type 1 Diabetes can be less stringent than in Type 2 Diabetes. With the mastery of calculating mealtime carbohydrate exchanges (discussed later in the article), patients can eat almost anything, adhering to the principles of rational nutrition directed to the general healthy population. It is recommended to eat in a varied, balanced way, individually tailored to the patient, and based on foods with a low glycemic index (GI).
Nutritional Recommendations of the Polish Diabetes Association for Patients with Type 1 Diabetes (2019)
Carbohydrates – there is insufficient scientific evidence to determine one optimal amount of carbohydrates in the diet. A change in the carbohydrate content from 55% to 45% of the diet is well received. For people with high physical activity, their share can be increased to 60%. It is recommended to choose carbohydrates with a low GI and high fiber content, as well as to limit simple carbohydrates, added sugars, sweet snacks, and sweetened juices. The daily fructose intake should not exceed 50 grams.
Proteins – the amount of protein in the diet should be determined individually. It should be 15-20% and correspond to 1-1.5 g/1 kg of body weight per day. There is no need to limit animal protein, but for patients with Type 1 Diabetes, the Mediterranean diet may be beneficial, with an increased proportion of fish and plant protein.
Fats – the share of fats in the diet can be the same as in a healthy person and range from 25% to 40%. Attention should be paid to the type of fats. Saturated fats should not exceed 10% of the dietary energy value. Monounsaturated fats up to 20% of the dietary energy value and polyunsaturated fats from 6 to 10% of the dietary energy value.
Fiber – the recommended amount of fiber is about 15 g/1000 kcal, and it is advised to increase the amount of resistant starch
Vitamins and Minerals – Supplementation of vitamins or micronutrients in patients without identified deficiencies is not necessary, except for vitamin D3, which should be supplemented according to general population recommendations and its levels should be monitored biochemically every 6 months. In patients with identified nutritional deficiencies, appropriate supplementation should be introduced under specialist control. One of the tests that allow for precise and non-invasive determination of elemental levels in the body is Elemental Hair Analysis (EHA).
Salt – the amount of salt from all sources should not exceed 5 grams per day.
METHODS OF TREATMENT AND THERAPY
Type 1 Diabetes cannot be cured. It can only be managed through continuous insulin therapy and glycemic control. The goal of diabetes treatment is to achieve normal glycemic values expressed in HbA1C control tests, not exceeding 7.0%. Additional examinations performed to monitor the treatment include blood pressure measurements, complete blood count with lipid panel, and body weight control.
INSULIN THERAPY
The key element in Type 1 Diabetes therapy is insulin therapy. The state of normoglycemia can be achieved by replicating basal insulin levels and its meal-related increases. Methods of intensive insulin therapy are divided into: personal insulin pump therapy model and insulin pen therapy model. Insulin therapy involves the external administration of all-day insulin, so-called “basal” and “bolus” insulin.
Long-Acting Insulin – “Basal”
“Basal” insulin aims to protect the body from glycemic fluctuations throughout the day. Glycemic fluctuations are influenced not only by consumed food but also by a range of processes occurring in the body. In insulin pen therapy, long-acting insulin, an analogue of human insulin with a typically 24-hour duration of action depending on the preparation, is used. This means that patients administer a given number of units of long-acting insulin once a day at a specified time, usually intramuscularly (thigh/arm) or in the abdominal wall. The initial amount of long-acting insulin units is determined by the treating diabetologist. These doses are often modified by patients based on their own observations of glycemic fluctuations, which are influenced by many factors.
Short-Acting Insulin – “Bolus”
In personal insulin pump therapy, instead of long-acting insulin, short-acting insulin (the same as that administered for meals) is given in hourly subcutaneous injections of small doses. The doctor or experienced patient programs the daily basal profile in the insulin pump by entering a given amount of injected insulin in hourly doses. This method is more precise than pen-based basal administration and allows for more modifications in the profile of such a “base”. The dose of short-acting insulin is determined based on the consumed meal. Calculated boluses include simple, extended, and combined. In pen-based insulin therapy, only simple boluses can be administered. In personal insulin pump therapy, both simple, extended, and combined boluses are possible.
HOW TO CALCULATE THE INSULIN DOSE FOR OUR CHILD?
The ability to correctly estimate the insulin dose for a meal is the most difficult and important element of therapy in Type 1 Diabetes. The level of education provided in hospital centers across Poland varies greatly, so verifying this skill in the patient or their caregiver, as well as helping in learning the correct calculation of exchanges, often rests on the dietitian treating the patient.
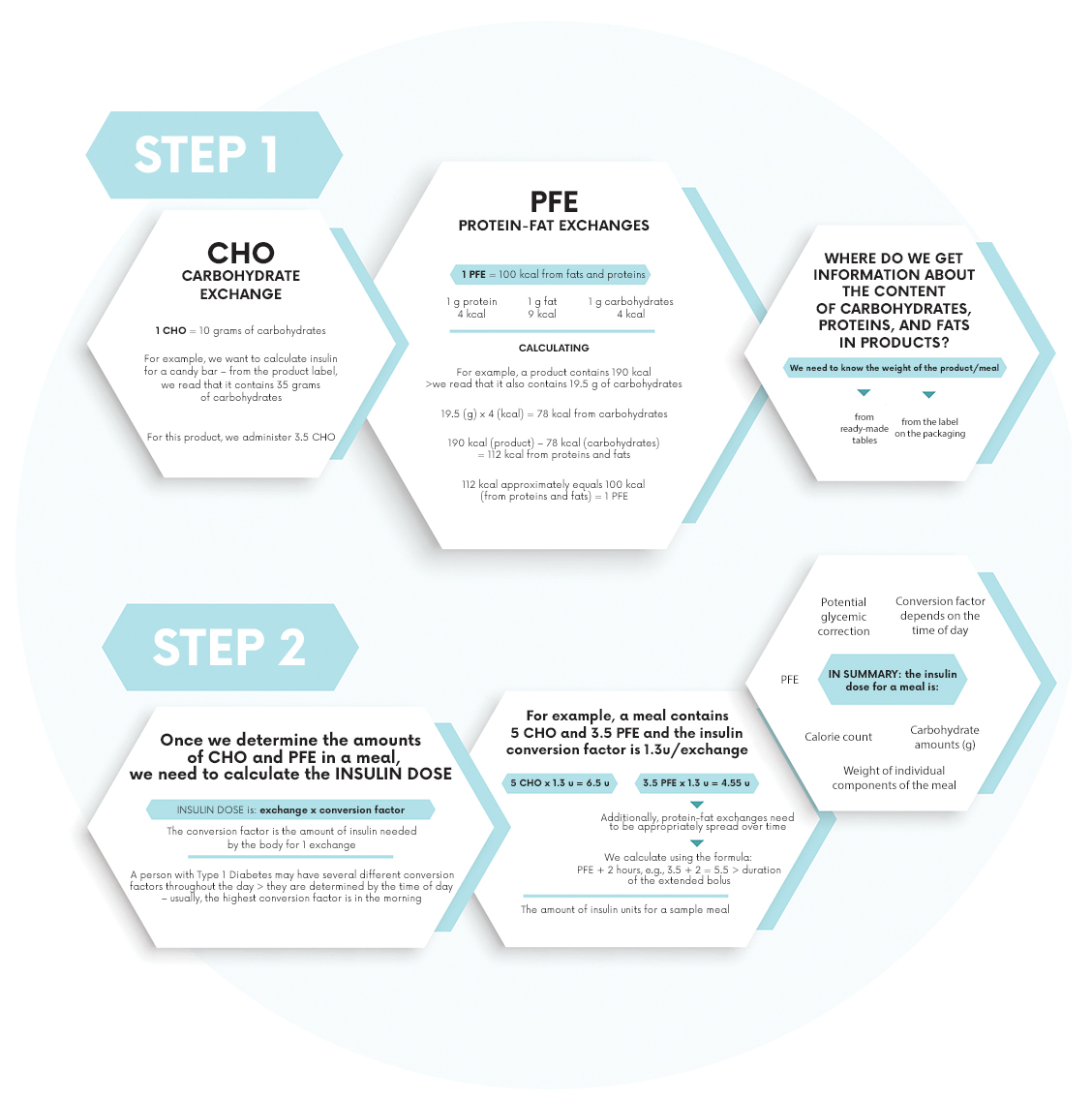
To determine the correct dose of insulin, meals should be converted into carbohydrate exchanges (CHO) and protein-fat exchanges (PFE). 1 carbohydrate exchange is the amount of food that contains 10 g of carbohydrates. 1 protein-fat exchange is the amount of product that contains 100 kcal from proteins and fats. The method of calculating CHO and PFE exchanges and converting them into units of administered insulin is presented below.
Carbohydrate Exchange (CHO) – Amount of product containing 10 g of carbohydrates.
Protein-Fat Exchange (PFE) – Amount of product containing 100 kcal from proteins and fats.
Special smartphone applications are extremely helpful in calculating the correct insulin doses. One such application is VitaScale, which automatically calculates the exchanges, and after entering specialized settings, also the ready insulin doses.
GLYCEMIC CONTROL
Another key aspect of Type 1 Diabetes control is measurement, i.e., self-monitoring of glycemia. It can be done using a traditional strip glucometer or through modern Continuous Glucose Monitoring (CGM) systems. Normoglycemia in Type 1 Diabetes is considered to be a range from 70 mg/dl to 180 mg/dl.
Most important glycemic measurements:
- The first fasting measurement, after waking up,
- Measurement before each meal,
- Measurement before sleep,
- At least 2 measurements at night,
- Measurement before starting physical activity,
- Measurement after finishing physical activity,
- Measurement when feeling unwell and experiencing symptoms of hypoglycemia or hyperglycemia.
- pomiar przy złym samopoczuciu i występowaniu objawów hipoglikemii lub hiperglikemii.
As the course of the disease is very variable and dynamic, practically everything can affect the glycemic levels and individual insulin doses throughout the day, starting from the patient’s age and physical effort, through the type of meal to the weather, outside temperature, even strong wind, stress, excessive excitement, or fear. The greatest threats from insulin therapy are hypoglycemia and hyperglycemia, as well as disease complications.
HYPOGLYCEMIA
Hypoglycemia, or low blood sugar, is too low a glucose concentration in the blood. It is considered hypoglycemia when the glucose level falls below 50 mg/dl (in children < 70 mg/dl). Its causes can vary, with the most common in Type 1 Diabetes being the administration of too large an insulin dose and excessive physical exertion. Hypoglycemia can lead to loss of consciousness and even death.
In severe hypoglycemia, caused by a very low blood sugar concentration with the symptom of loss of consciousness, GlucaGen is used. The injection kit contains a single dose of biosynthetic human glucagon (0.001 g) and a syringe with a solvent and can be easily stored at home, at work, or at school. Glucagon causes the release of glucose stored in the liver and quickly raises its level in the blood. It is effective whether administered intravenously, intramuscularly, or subcutaneously. Treatment should be supplemented with oral carbohydrate administration.
In the event of hypoglycemia, immediate action is necessary!
1. Administer glucose to the patient, e.g., in the form of juice.
2. Wait a moment and check if the sugar level rises. If not – administer glucose again.
3. If unconsciousness occurs, call an ambulance and administer GLUCAGEN, an injection containing glucagon.
HYPERGLYCEMIA
Hyperglycemia, or high blood sugar, is an excessively high glucose concentration in the blood. It is considered hyperglycemia when the glucose level exceeds 180 mg/dl. In patients with Type 1 Diabetes, glucose levels of 200-300 mg/dl (and more) are very common. The most common causes of hyperglycemia include administering too small an insulin dose or errors in its administration (e.g., insulin leakage – when using a pen or occlusion of the insertion site – when using a pump).
Basic knowledge about how to feed, how to properly administer insulin, and what specific glycemia measurement results mean is essential and mandatory for all parents of children with Type 1 Diabetes. Although calculating carbohydrate and protein-fat exchanges and insulin doses may seem complicated, through thoroughness and experience, everyone can master this skill to ensure safety for their child and to feel more confident in this difficult situation.
Proper Management in Case of Hyperglycemia:
1. Administer a specially calculated correction dose of insulin, ensuring that technical errors are excluded.
2. Wait an hour and measure glycemia again to make sure its level is already dropping.
3. . IMPORTANT! Never administer corrections more frequently than every 2-3 hours!
There are many more aspects related to diabetes in children, and the knowledge and skills that caregivers must possess are very extensive. Issues of caring for sick children in educational institutions, topics of dangers arising from the disease, psychological aspects related to pain and rebellion against the disease, and many other problems, are daily concerns for many families throughout Poland. One of many serious issues associated with Type 1 Diabetes is also comorbid diseases.
Magdalena Jerzak – Diet.Point nr 2(5)/2020; 4-11
Bibliography:
1. 2019 Guidelines on the managment of diabetic patients. A position of Diabetes Poland. Clinical Diabetology 2019.
2. Rachel Besser, “Diabetes in Children – On the Other Side of the Mirror,” published by MADA, Warsaw 2013.
3. Karolina Klewaniec-Wypychacz, Marcin Wypychacz, Przemysław Jarosz-Chobot [eds.], “Type 1 Diabetes – Family Diabetic Guide,” published by PZWL, Warsaw 2019.
4. Clinical recommendations for the management of patients with diabetes 2015, Polish Diabetes Association, Volume 4, Supplement A.”
5. Ragnar Hanas, “Type 1 Diabetes in Children and Adolescents,” 2010, 2nd edition.
6. Elżbieta Piontek, Daniel Witkowski, “Diabetes in Children,” PZWL publishing house, Warsaw 2009.